Parathyroid Disorders: Causes, Symptoms, and Treatment Options
Some individuals suffer from disorders of the parathyroid glands, such as hyperparathyroidism or hypoparathyroidism, which can lead to symptoms including muscle cramps, irregular heartbeats, and weakened bones. But what exactly are the parathyroid glands? What are the most common disorders that affect them? And how are these conditions treated?
What Are the Parathyroid Glands?
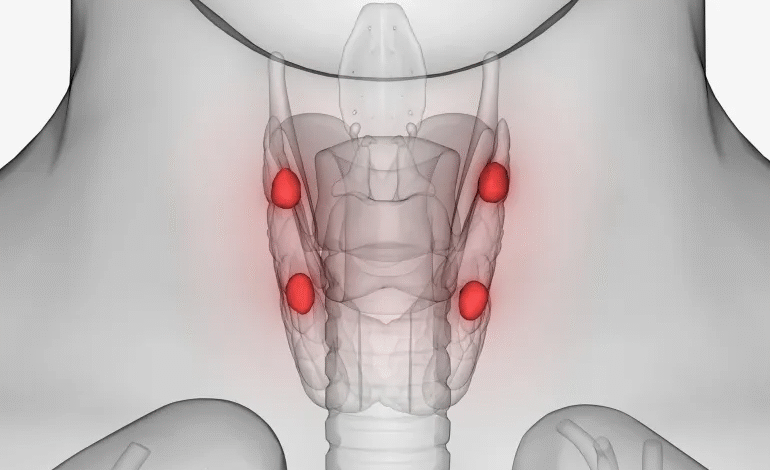
The parathyroid glands are tiny endocrine glands located behind the thyroid gland in the neck. They secrete parathyroid hormone (PTH), which plays a crucial role in regulating calcium levels in the blood and bones.
According to Dr. Fawzat Al-Shanq, a consultant in endocrinology and diabetes, the parathyroid glands—commonly four in number—are no larger than a grain of rice, weighing approximately 30 mg in men and 35 mg in women. These glands regulate calcium balance in the body by influencing bones, kidneys, and the intestines.
Common Parathyroid Disorders
Disorders of the parathyroid glands typically fall into two categories: hyperparathyroidism (overactivity) and hypoparathyroidism (underactivity).
Hyperparathyroidism
Dr. Al-Shanq explained that hyperparathyroidism can result from various causes, including:
- Low blood calcium levels due to vitamin D deficiency
- Poor dietary calcium intake or malabsorption in the intestines
- Kidney dysfunction or medications that affect calcium metabolism
- A benign tumor or glandular enlargement (hyperplasia)
- Rarely, a genetic disorder such as multiple endocrine neoplasia (MEN)
These conditions lead to an overproduction of PTH, which raises calcium levels in the blood and can cause serious complications.
Hypoparathyroidism
In contrast, hypoparathyroidism often results from:
- Neck surgeries, particularly thyroidectomy or cancer treatments
- Autoimmune diseases, where the immune system attacks the glands
- Congenital absence of the glands
- Low magnesium levels, which impair hormone secretion
- Exposure to radiation therapy or radioactive iodine treatment
Symptoms of Parathyroid Disorders
Dr. Al-Shanq outlined the symptoms associated with both conditions:
Hyperparathyroidism may cause:
- High blood calcium levels
- Bone fragility and fractures
- Kidney stones
- Fatigue, joint and bone pain
- Dehydration, excessive thirst and urination
- Irregular heart rhythms
- Cognitive and neurological disturbances
Hypoparathyroidism often leads to:
- Low calcium and high phosphate levels
- Tingling or numbness in lips and fingers
- Muscle cramps, especially in the hands and face
- Brittle nails, dry skin, hair loss
- Anxiety, depression, and menstrual irregularities
Diagnosis and Investigations
Diagnosis begins with a clinical examination, often revealing signs like muscle spasms. Laboratory tests confirm abnormal calcium, phosphate, magnesium, and PTH levels. In hyperparathyroidism, labs typically show high PTH and calcium with low phosphate and elevated alkaline phosphatase (ALP). Imaging such as ultrasound or sestamibi nuclear scan helps detect tumors or gland enlargement.
Treatment Approaches
Dr. Al-Shanq emphasized that untreated parathyroid dysfunction can result in severe complications including seizures, osteoporosis, heart arrhythmias, and kidney failure.
For hyperparathyroidism, surgery to remove the affected gland is the preferred treatment. If surgery isn’t possible, Cinacalcet may be prescribed to reduce hormone levels.
Hypoparathyroidism is managed with:
- Calcium supplements
- Active vitamin D (e.g., Alfacalcidol)
- In rare cases, recombinant PTH injections, though expensive, are effective
Early diagnosis and timely intervention are critical in preventing long-term health issues.
Surgical Perspective: When Is Surgery Needed?
According to Dr. Suhail Youssef Bakkar, a specialist in thyroid and endocrine surgery, primary hyperparathyroidism—often caused by a benign tumor in one gland—is the most common form requiring surgery.
In about 90% of cases, only one gland is affected, while two glands are involved in 5–7% of patients. Rarely, all four glands are affected due to glandular hyperplasia.
“In primary hyperparathyroidism, medication is generally insufficient. Surgical removal of the affected gland is the definitive treatment,” Dr. Bakkar explained.
Advances in Surgical Techniques
Surgical methods have greatly advanced. Traditional open surgery involving full neck exploration has largely been replaced by minimally invasive procedures, made possible through ultrasound and nuclear imaging, which can locate the problematic gland with up to 85% accuracy.
“We can now perform the surgery through a small cosmetic neck incision or even endoscopically via the mouth or neck,” Dr. Bakkar noted. “This reduces scarring and speeds up recovery significantly.”
Success rates exceed 98%, especially when performed by experienced surgeons. Complications are rare but may include:
- Temporary hoarseness due to vocal cord nerve irritation (less than 1%)
- Bleeding (very rare)
- Temporary drop in calcium (known as “hungry bone syndrome”)
Recovery and Follow-Up
Patients undergoing minimally invasive surgery can often return to normal life within two days, provided calcium levels remain stable.
Postoperative care includes:
- Monitoring calcium levels
- Temporary use of calcium and vitamin D supplements
- Regular checks on kidney and bone function
Recurrence is uncommon except in rare hereditary cases, which might require future surgeries.
“This is one of the few surgeries where patients experience immediate relief, especially from bone pain and mental fog,” Dr. Bakkar said. “The improvement is often noticeable as soon as the patient wakes up from anesthesia.”